Bridging the gap between policy, technology, and the lived experiences of those who rely on essential services.
The aged and disability care sector was undergoing significant transformation. New policy reforms, rapid technological shifts, and the increasing complexity of user needs were placing unprecedented pressure on care providers. Telstra Health recognised that bridging the gap between policy, technology, and lived experience was essential to delivering better outcomes for both care recipients and care providers.
I was engaged to lead a service design initiative that could navigate this complexity and deliver measurable benefits.
Client
Telstra Health
Role
Experience Manager
Services
Research & Insights
Service Design
Responsibility
Managed and planned the research approach to provide actionable, viable solutions during a sector-wide transformation.
Long-Term Strategy & Shaping The Vision
Strategic Alignment and Vision Setting
I began by running multi-disciplinary strategy workshops with product, engineering, marketing, and policy teams. These sessions clarified the organisation’s aspirations, identified critical user and business needs, and defined what success would look like in measurable terms.
Understanding Lived Experiences
I conducted in-depth ethnographic research with a diverse range of participants — from elderly individuals receiving daily in-home support to occupational therapists, nurses, and respite coordinators.
Mapping the System
Multiple high level ecosystem maps was developed to visualise the interactions between patients, carers, providers, and support services. This revealed hidden operational gaps, complex hand-offs, and areas where policy and technology were out of sync with user needs.
Reconciling the Ideal vs the Real
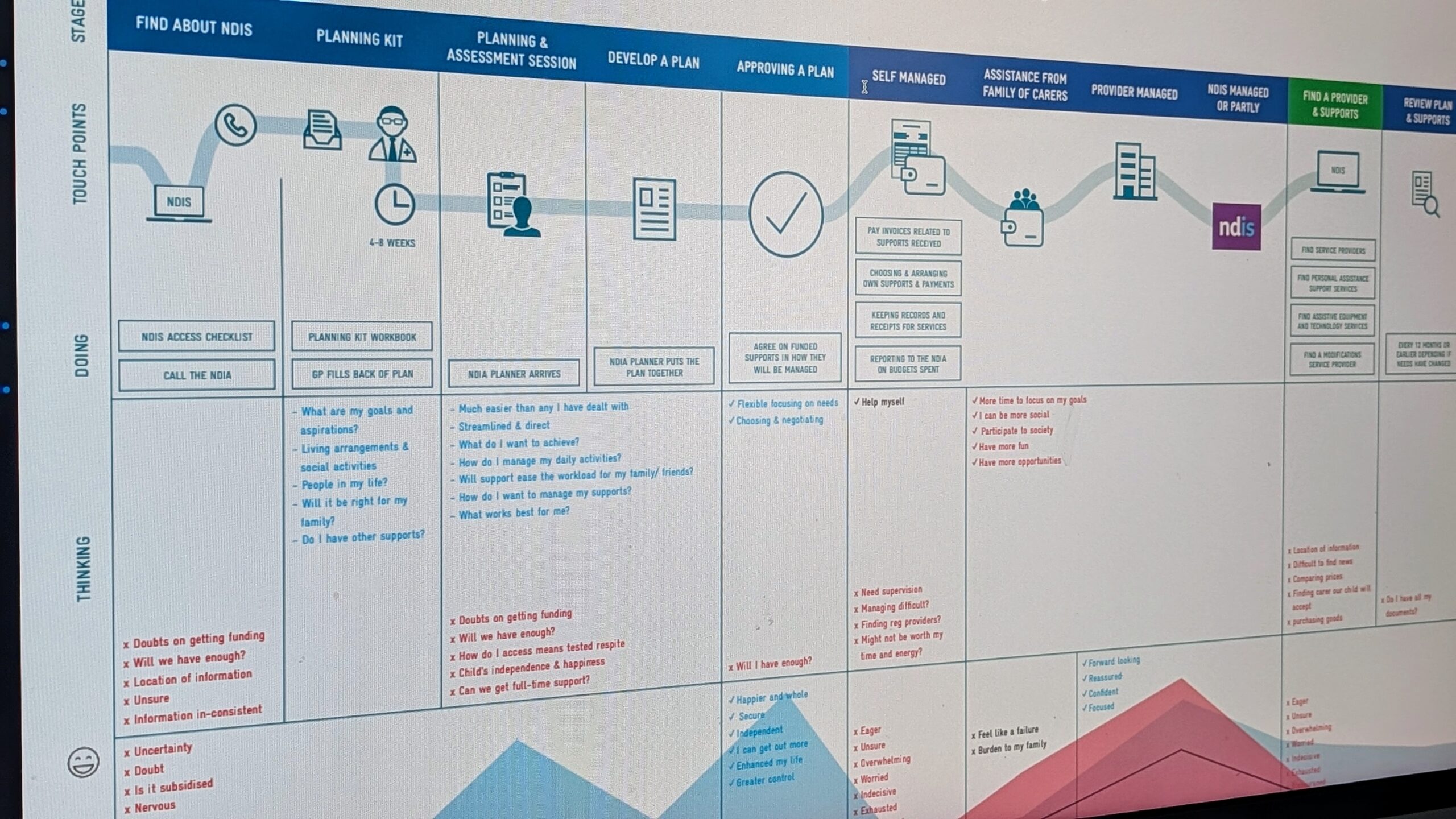
Investigating the NDIS Journey
To deepen our understanding of the systemic barriers facing care recipients, I conducted targeted desktop research to explore how individuals with disabilities access support through the NDIS. This involved analysing: Official NDIS resources, application flows, and eligibility documentation First-person accounts shared in public forums, social media, and community blogs Broader commentary from advocacy organisations, media outlets, and inquiries The intent was to compare the “on-paper” experience presented by the NDIS with the frustrations, confusion, and delays voiced by real participants navigating the system. This contrast allowed us to ground our service concepts in the realities of approval processes, funding uncertainty, and language complexity, rather than designing solely around theoretical policy pathways. It also helped shape communication flows, support touchpoints, and digital onboarding steps that better aligned with user capability and expectations.Activity Summary
Approach to Gaining Insights
To deeply understand the challenges and needs within aged and disability care, we conducted in-depth ethnographic interviews with a diverse range of participants, including:
Care recipients: Individuals with chronic illnesses, disabilities, and elderly individuals requiring support at home.
Care providers: Support workers, nurses, general practitioners, occupational therapists, and respite coordinators.
Each session involved:
Contextual home visits
Observing participants in their living environments to understand daily routines, challenges, and workarounds.
Semi-structured interviews
Gathering qualitative insights through open-ended questions.
Raw data analysis
Examining tools and technologies participants use to manage their care.
Thematic synthesis
Identifying common patterns and divergences across participant experiences.
Physical Artifacts for Participant Collaboration
To engage participants effectively and capture detailed insights, I utilized physical artifacts that facilitated interaction and collaboration. These included:
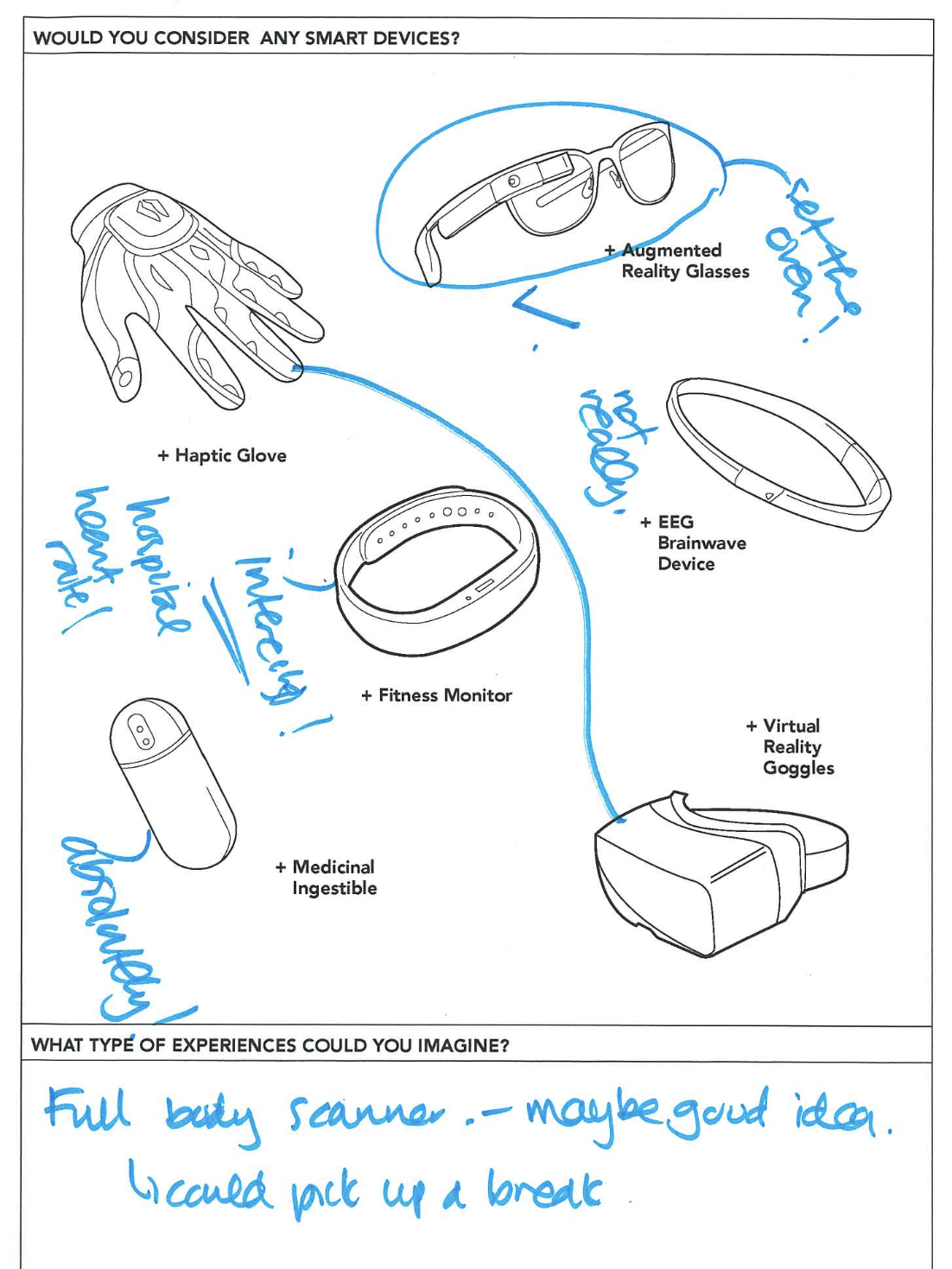
Health Devices
A tool to explore participants' openness to innovative health technologies and their potential use cases. This allowed participants to visualize and articulate their preferences and hesitations about adopting new technology.
About My Home
A worksheet designed to capture participants’ emotional and practical connections to their living spaces, including frustrations and ideal changes. This helped uncover deeper sentiments about their homes.
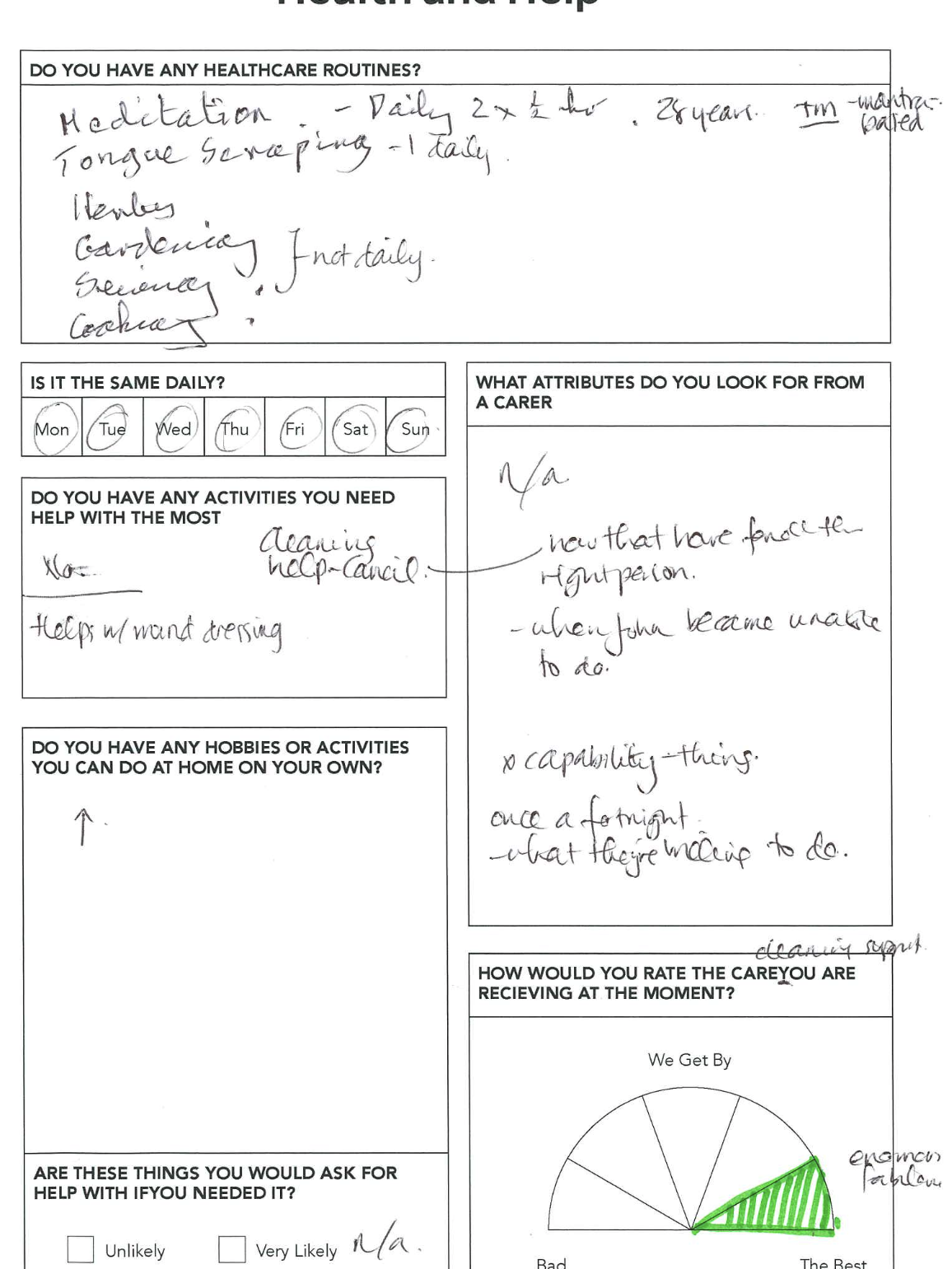
Health and Help
A structured form capturing participants' healthcare routines, required assistance, and expectations from carers. This revealed critical insights into daily struggles and support needs.
A Day in the Life
A timeline exercise where participants detailed their daily schedules, highlighting services used, activities, and involved individuals. This provided a clear picture of their routines and opportunities for service optimization.
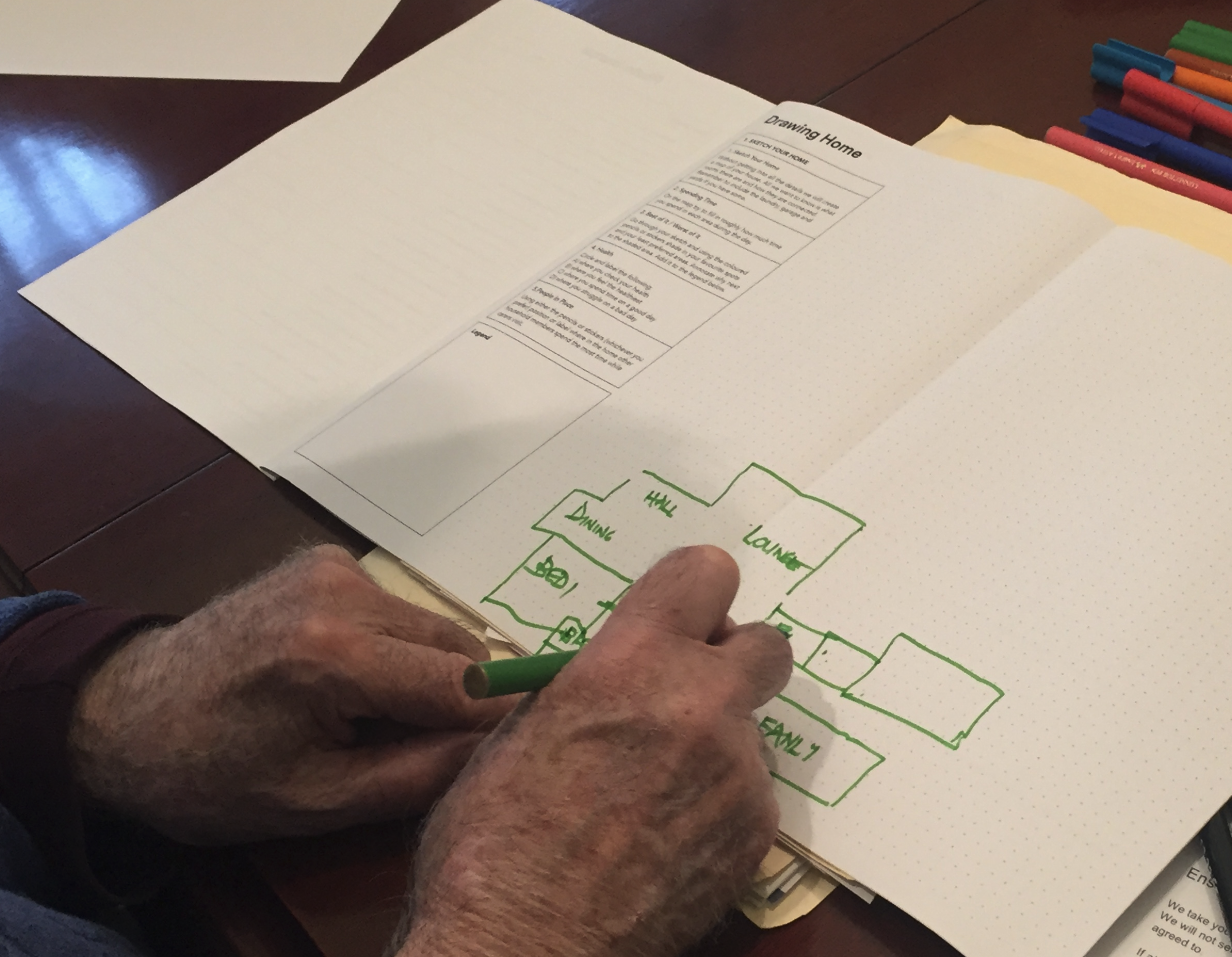
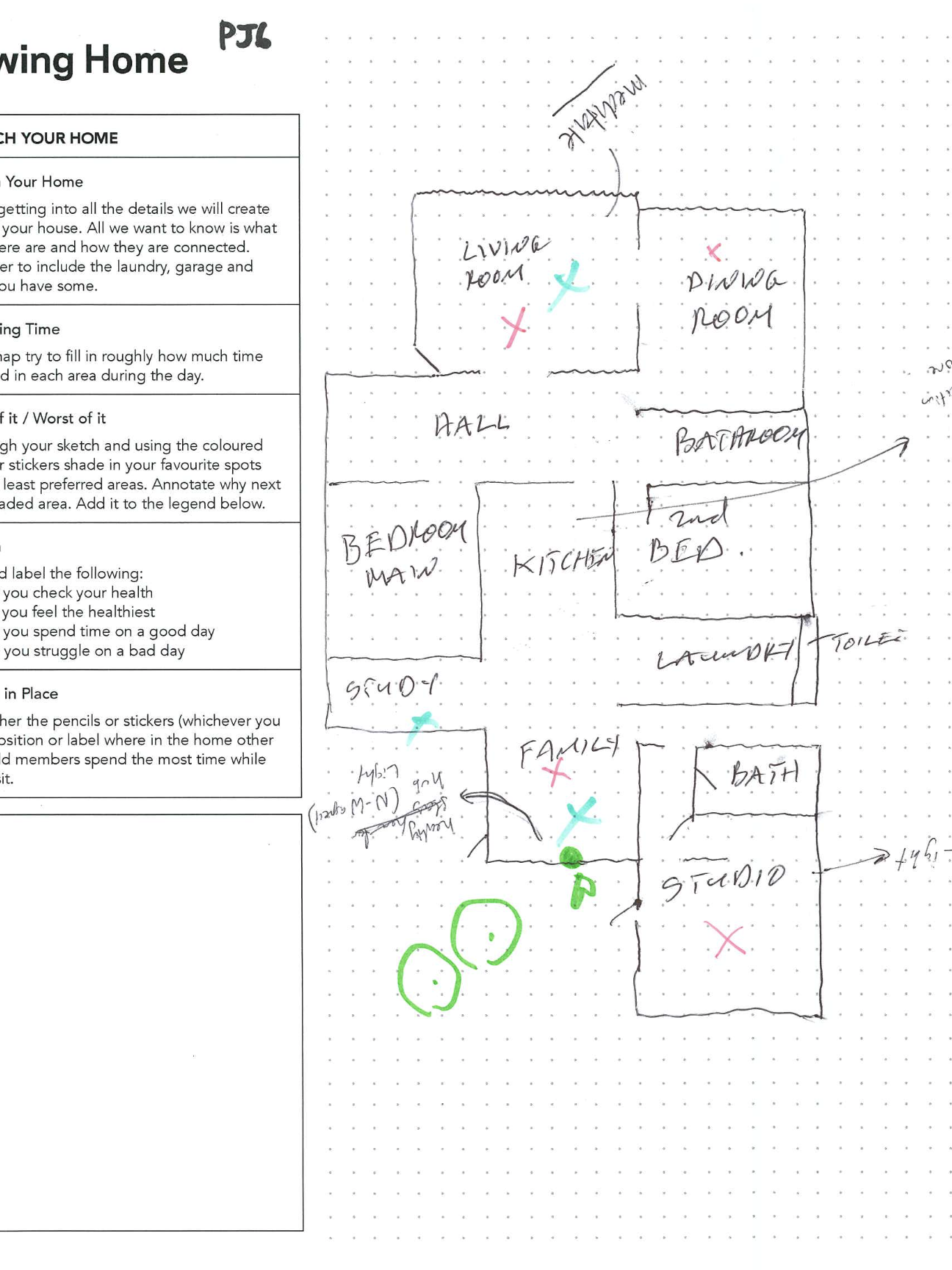
Drawing My Home
A home-mapping activity where participants sketched their living spaces and annotated areas of comfort, challenge, and interaction with carers illuminating the spatial dynamics of their environments and their impact on daily routines.
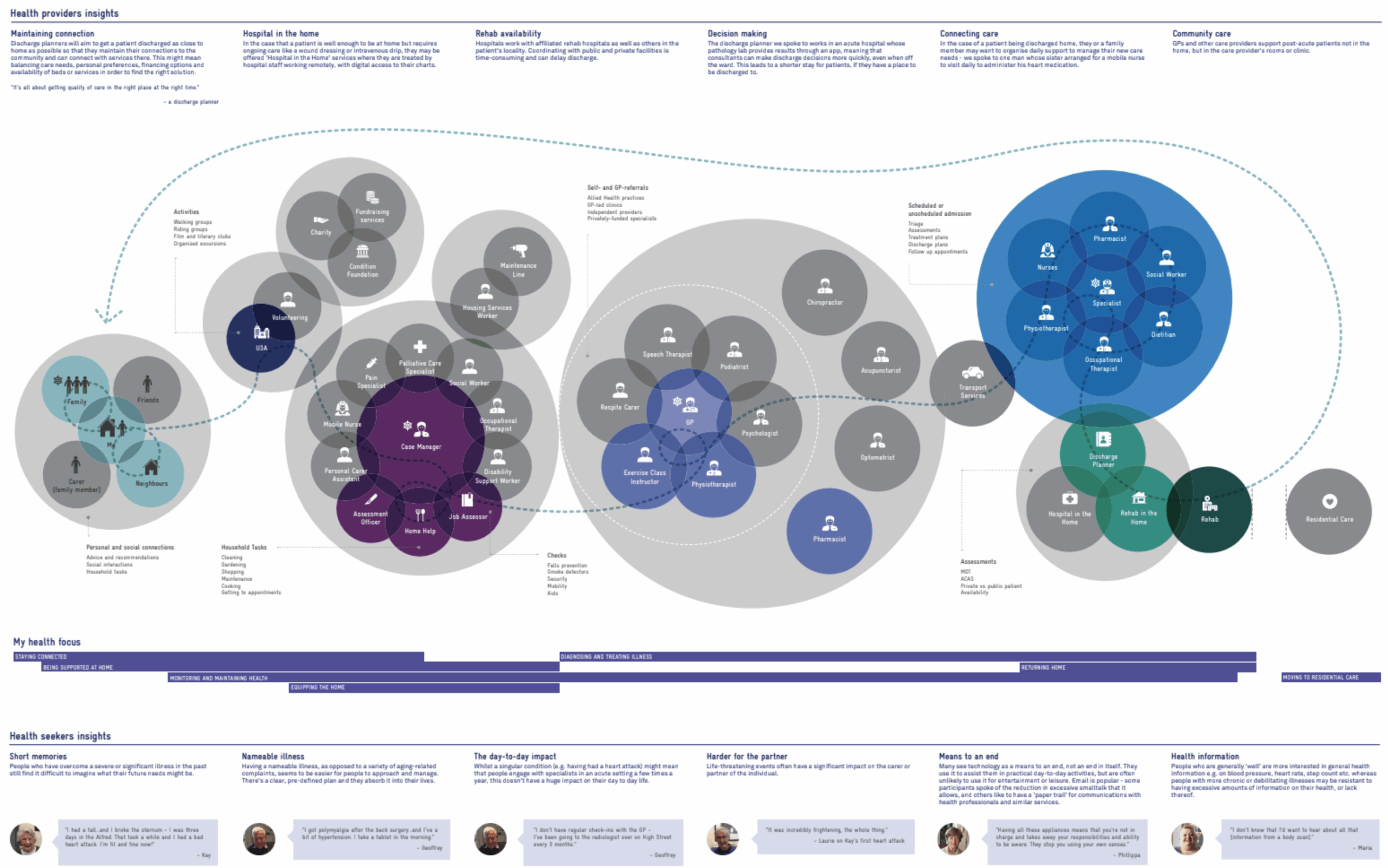
Eco-System Design
This ecosystem map is one of several service modelling artefacts developed to visualise how people navigate complex health and care services.
It draws directly from user research and stakeholder insights to reveal critical handoffs, service overlaps, and systemic gaps across the broader care journey.
By mapping interactions between patients, carers, providers, and support services, we surfaced the operational and emotional friction points that often go unseen. These insights informed both future-state experience models and cross-functional decisions around service design, product focus, and policy alignment.
Quantitative Validation
To complement our rich qualitative data, the team and I recognised the value of quantifying how widespread certain challenges were, particularly around service navigation, breakdown points, and perceived system clarity.
Service Navigation Confidence & Breakdown Survey
Goal:To quantify how confident people are navigating healthcare and support services, where they experience drop-offs or delays, and how these correlate with specific service types or life stages.What it Measured:
Outcomes & Impact
The data helped to identify: Quantify friction points across the ecosystem map to support prioritisation Cluster insights by user type and support need to inform service differentiation Strengthen stakeholder engagement by providing statistical evidence alongside personal narratives Support investment decisions around digital tools, triage models, and staff capability building This survey was designed to scale insight gathering across a broader segment and bring evidence-backed clarity to design decisions—ensuring we weren’t just solving for the loudest voice, but for the most common and critical needs.
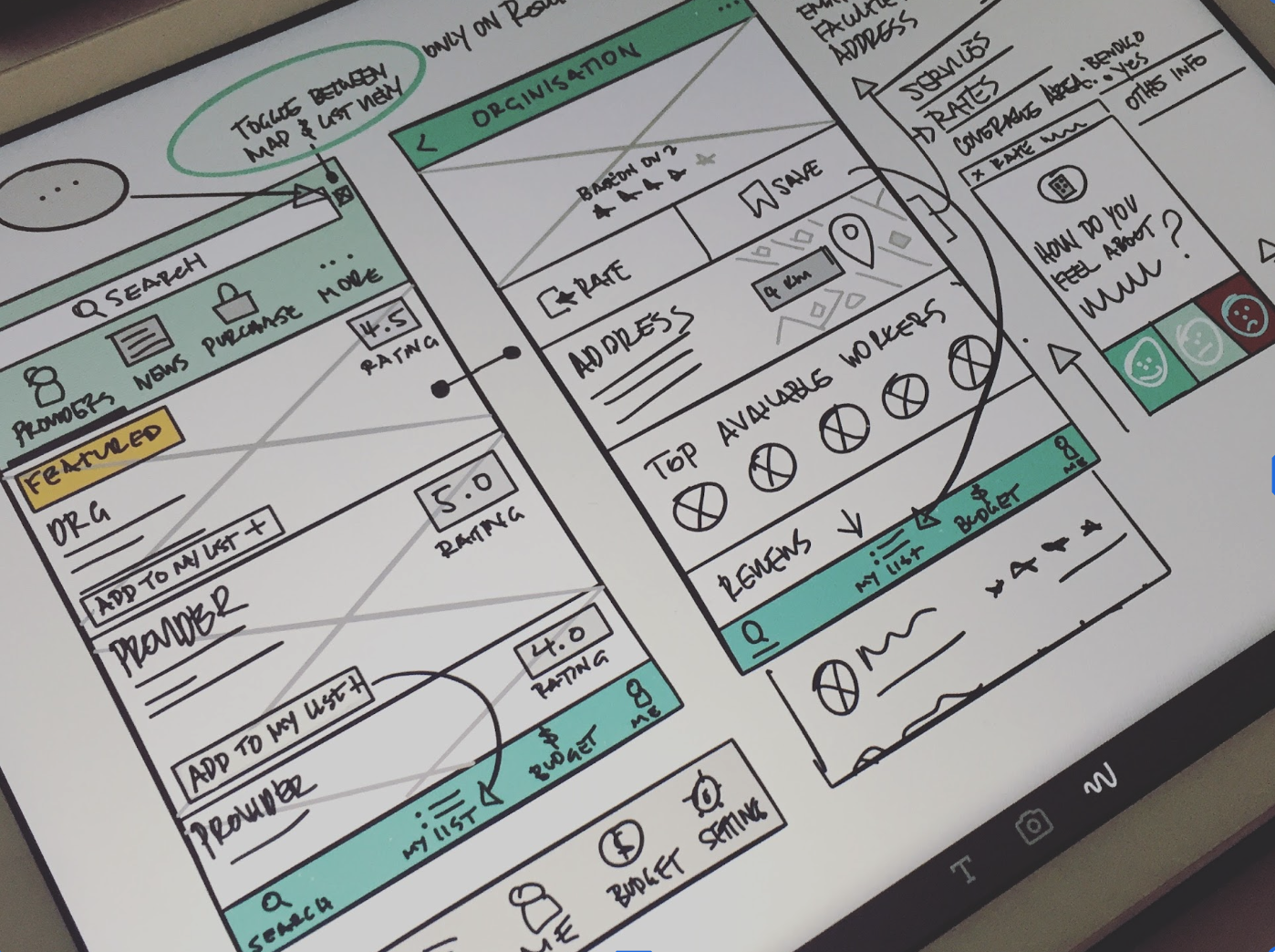
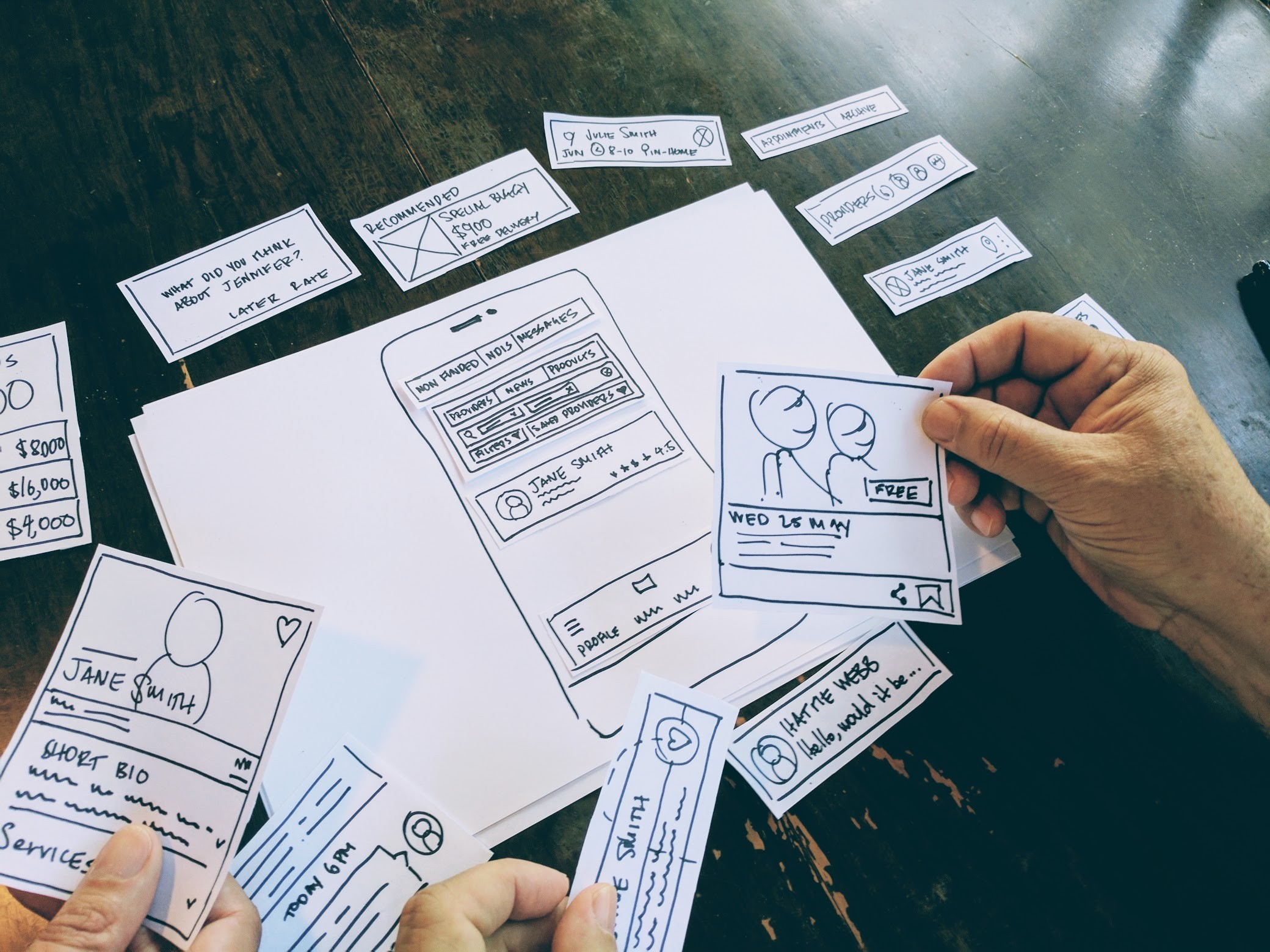
Prototype and testing service concepts
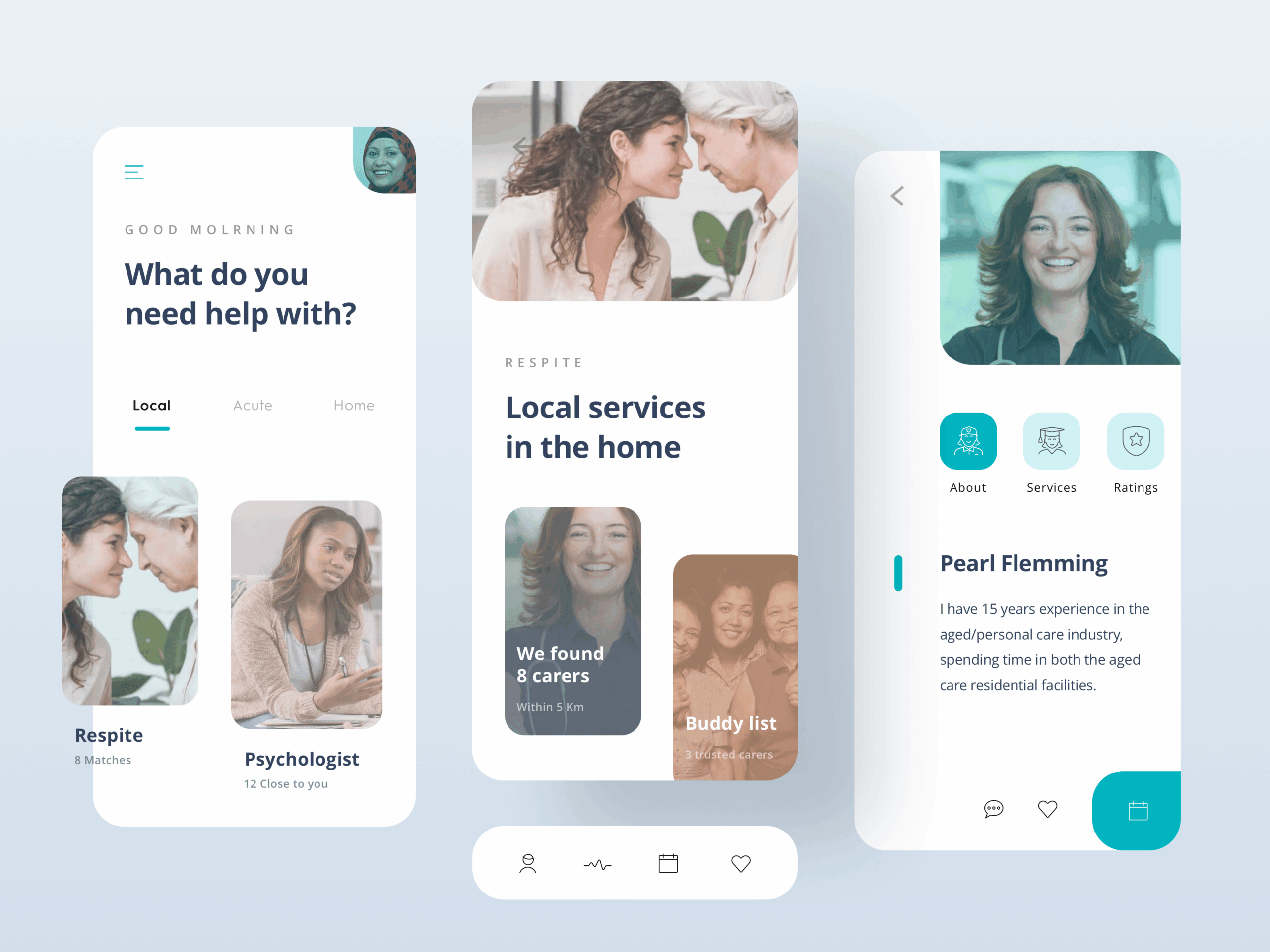
Yes, these are my designs.
Early Concept Validation
Used to explore early ideas with real users and stakeholders through lightweight, human-centred experiments helped co-design future-state experiences, identify unmet needs, and test desirability before committing to detailed design or build.
High-Fidelity MVP Testing
Built to simulate real-world interaction across digital and organisational layers.
These higher fidelity prototypes were used to test functionality, language, flows, and service viability—providing clear data to inform platform, engineering, and operational decisions.
Validating Adoption & Alignment
Combined insights from both lo-fi and hi-fi testing to measure potential for adoption—balancing customer needs, brand context, operational capability, and commercial viability.
⸺ Qualitative Research
Leverage agile frameworks to provide a robust synopsis for high level overviews. Iterative approaches to corporate strategy.
⸺ Sketch Visualization
Organically grow the holistic world view of disruptive innovation via workplace diversity and empowerment everyday routines.
⸺ Engineering Strategy
Leverage agile frameworks to provide a robust synopsis for high level overviews. Iterative approaches to corporate strategy.
⸺ Rapid Prototyping
Organically grow the holistic world view of disruptive innovation via workplace diversity and empowerment everyday routines.
⸺ CMF Specification
Leverage agile frameworks to provide a robust synopsis for high level overviews. Iterative approaches to corporate strategy.
⸺ Product Packaging
Organically grow the holistic world view of disruptive innovation via workplace diversity and empowerment everyday routines.
Product Delivery & Impact
At the conclusion of this engagement, our cross-functional work culminated in the delivery of an MVP product for care matching—a streamlined platform designed specifically for carers and care coordinators to reduce mismatch and improve continuity of care.
Monitoring & Review
Quarterly reviews of KPIs with Telstra Health leadership. Feedback loops via surveys and coordinator interviews to refine matching algorithms and workflows. Annual impact assessment to evaluate sustained improvements and policy alignment.
Realised Impact (Pilot Rollout)
-
Significant reduction in carer–recipient mismatches and service cancellations.
-
Increased satisfaction reported by care recipients and staff.
-
Improved scheduling efficiency and reduced manual rework.
-
Strengthened case for broader investment in digital coordination infrastructure.